A dangerous and drug-resistant fungus is evolving to become more infectious and is now spreading across the globe, a major scientific review has warned. The pathogen, Candida auris, presents a severe threat, particularly to those with weakened immune systems, and is associated with mortality rates exceeding 50% even with treatment.
A Global Pathogen with Unique and Dangerous Traits
First identified in 2009 in a patient's ear canal in Japan, Candida auris has since been detected in at least 61 countries across six continents. It was flagged as a major public health threat in India as early as 2014. The latest research, published in Microbiology and Molecular Biology Reviews, highlights several alarming characteristics that explain its rapid spread.
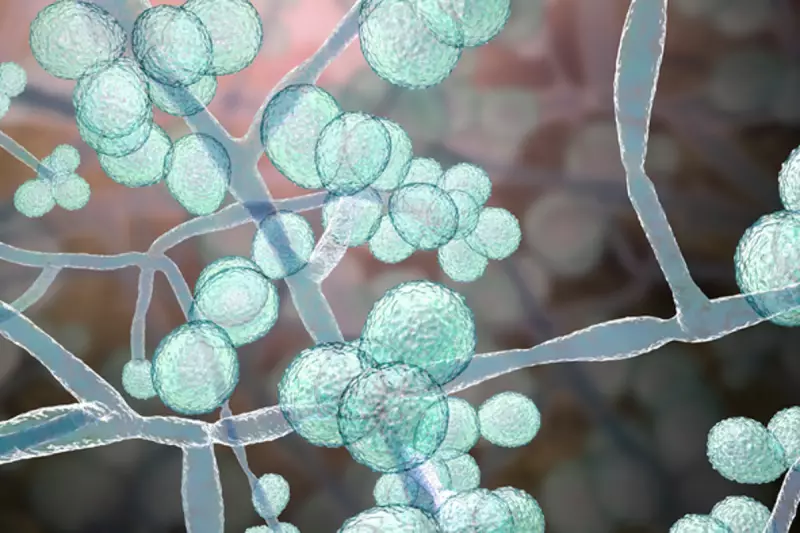
The fungus possesses a remarkable ability to switch its growth form, moving from a yeast-like state to a filament-driven mode that aids its spread. Furthermore, it has specialised cell wall proteins that allow it to adhere to human skin "like glue," facilitating colonisation. This skin colonisation is a critical concern in healthcare settings, as colonised patients can unknowingly transmit the infection to others within and between hospitals.
Evading Treatment and Diagnosis
The study outlines the sophisticated ways Candida auris resists antifungal drugs. Its cell membrane is equipped with "efflux pumps" that actively remove medicinal compounds before they can work. The fungus also clusters together to form slimy, protective biofilms on surfaces, creating a barrier that drugs struggle to penetrate. Researchers acknowledge that other, as-yet-unknown resistance mechanisms may also be at play.
Compounding the treatment challenge is the difficulty in diagnosis. The infection is frequently misidentified, leading to dangerous delays in administering the correct antifungal therapy. This diagnostic hurdle allows the infection to gain a stronger foothold in patients.
An Urgent Call for Action and New Solutions
The scientific review concludes with a stark warning and a call for a coordinated global response. It underscores the pressing need to develop novel, broad-spectrum antifungal agents, improve diagnostic tests, and explore immune-based therapies and vaccines for high-risk patients.
The authors stress that improved surveillance and awareness are vital, especially in resource-poor nations where tracking outbreaks can be difficult. There is a glimmer of hope, however, as the review notes that three new drugs currently in clinical trials may soon become available to help combat this formidable fungal foe.





