Enfield's Measles Outbreak: All Infected Children Were Unvaccinated, Says GP
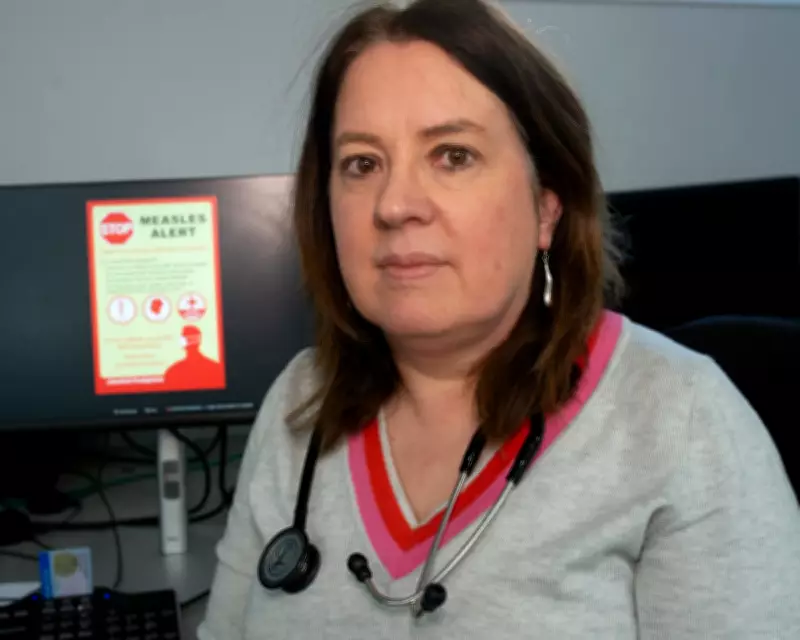
Health professionals in Enfield, north London, are confronting a significant measles outbreak, with Dr Phillipa Vincent of Carlton House Surgery revealing that all children infected in the borough had not received the MMR vaccine. This alarming situation underscores a persistent public health challenge in the area, where low vaccine uptake has been exacerbated by factors such as misinformation, deprivation, and community distrust.
Ongoing Public Health Efforts
Dudu Sher-Arami, Enfield Council's director of public health, described the outbreak as unsurprising given years of struggling to improve vaccination rates. She emphasized that working with communities to encourage vaccinations remains an "ongoing public health challenge," particularly in areas like Edmonton, which is at the epicentre of the outbreak and faces high levels of deprivation.
Sher-Arami explained that for many residents, vaccination is not a priority due to issues like multiple jobs, low income, and insecure housing. Additionally, the "churn of the population" complicates efforts to maintain consistent immunisation coverage. In response, the council is intensively scouring databases to identify children who have missed jabs and contacting their parents, while also setting up special vaccination clinics in schools and increasing capacity at GP surgeries.
Challenges of Vaccine Hesitancy
Dr Vincent noted a rise in "vaccine hesitancy" within the community, partly fueled by the Covid-19 pandemic. She observed that concerns have shifted from outdated fears about autism to anxieties over vaccine contents, driven by misinformation from non-scientific groups on social media. Despite recent media coverage prompting a slight increase in vaccine demand, including among adults, uptake remains low, and the surgery has implemented measures to prevent unvaccinated children with symptoms from waiting rooms.
Parents outside Carlton House Surgery expressed mixed reactions, with some, like Pan, feeling secure due to their children's vaccinations, while others questioned the low uptake. Prof Azeem Majeed of Imperial College London highlighted that Enfield's demographic factors—such as ethnic diversity, lower education levels, and high mobility—intersect with online misinformation and distrust of authorities, contributing to the decline in vaccine uptake since 2012.
Innovative Solutions and Future Prospects
To address these issues, health professionals are exploring innovative approaches. Sher-Arami mentioned a government-funded pilot project that could enable health visitors to provide vaccinations, potentially improving access. Ronny Cheung of the Royal College of Paediatrics and Child Health advocated for expanding vaccine delivery roles and enhancing community engagement through trusted voices, noting that many so-called hesitant parents are receptive after informed conversations.
He also pointed out that access barriers, such as difficulty securing appointments and lack of prioritisation information, need addressing through better training for health workers. While media coverage of outbreaks can drive vaccination rates, official case numbers may be underestimates, underscoring the urgency of these efforts to prevent further spread.
Overall, Enfield's experience highlights the critical need for targeted public health strategies to combat measles and other vaccine-preventable diseases in an era of growing hesitancy and misinformation.





