A groundbreaking medical approach that slashes deaths from childbirth bleeding by 60% is being blocked from reaching tens of thousands of vulnerable mothers, following severe cuts to United States foreign aid initiated by the Trump administration.
A Medical Scandal and a Lifesaving Discovery
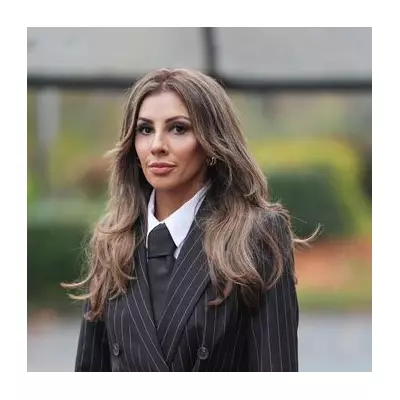
The journey to this breakthrough began over fifteen years ago for Professor Arri Coomarasamy, then a 38-year-old IVF trainee, after a harrowing visit to a Malawian hospital mortuary. He witnessed three deceased women, two of whom had bled to death after giving birth, a sight that propelled his career into tackling postpartum haemorrhage, the world's leading cause of maternal death.
Research led by Coomarasamy and the University of Birmingham uncovered a two-part "medical scandal": health workers were failing to diagnose half of all life-threatening bleeds in time, and treatments were being administered too slowly. The solution, proven in a 2023 trial, was transformative. It combined a simple plastic drape to accurately measure blood loss with the immediate, simultaneous administration of known effective treatments like oxytocin and tranexamic acid. This bundle of care reduced severe bleeding, surgeries, and deaths by an extraordinary 60%.
Funding Axe Falls on Critical Rollout
Just as this knowledge began to reach clinics in some of the world's poorest nations, a major funding source was severed. Following Donald Trump's sweeping cuts to foreign aid at the start of 2025, key US-funded programmes were dramatically scaled back. The 'Momentum Country and Global Leadership' initiative, dedicated to maternal and child health, was cancelled in over 10 of the roughly 25 countries where it operated.
Health workers who had seen the method's power now face a dire shortage of essential drugs and equipment, like the diagnostic drapes. "There is no doubt in my mind that the cuts have massively impacted the rollout," says Professor Coomarasamy, now at Oxford. Postpartum haemorrhage expert Cherrie Evans states plans to scale up training have "stalled," adding, "I feel like we're going back 20 years."
Lives Already at Risk in Malawi and Beyond
The consequences are starkly visible in Malawi, where Coomarasamy's mission began. Nurse Victoria Mzungu credits the new approach with saving a mother of twins who arrived at her clinic bleeding heavily. In the three clinics in Salima district using the method, no maternal deaths from bleeding were registered this year. Yet, since US funding ended, they lack key supplies.
The damage extends beyond direct treatment. Outreach programmes to remote communities have been cancelled, causing antenatal visit rates to fall. In Nkhotakota district, clinics lost track of 900 pregnant women and recorded over 2,000 fewer visits. Cases of excessive bleeding have jumped back to pre-2022 levels. An audit seen by The Independent concluded one woman's death from haemorrhage would have been preventable without the cuts.
Parallel work by WaterAid to ensure maternity wards had clean water and toilets has also stopped, deterring women from attending "dehumanising" facilities. A US State Department spokesperson said the administration is "prioritising direct investments in frontline healthcare workers" under its "America First Global Health Strategy," and is providing nearly $12m to Malawi for maternal and child health.
However, insiders warn the revised programmes now reach half as many countries and are restricted to "lifesaving interventions," excluding broader support like family planning. As Deborah Armbruster, a former USAID advisor, notes, solving maternal health crises is key to fixing entire health systems—a goal now pushed further out of reach.