In a major public health breakthrough, new gold-standard research has confirmed that the human papillomavirus (HPV) vaccine is dramatically effective at preventing cervical cancer. The findings, hailed as definitive, offer powerful evidence for the life-saving potential of this routine vaccination.
Definitive Evidence from Global Research
Two comprehensive new analyses from the prestigious Cochrane Institute, considered the benchmark for clinical research, have delivered clear and consistent results. The research found that girls vaccinated before the age of 16 were 80 percent less likely to develop cervical cancer later in life.
The vaccine, typically administered in two doses with the first given around age 11 and the second six to twelve months later, works by protecting against a group of sexually transmitted diseases caused by HPV. Cervical cancer is the fourth most common cancer among women globally, with approximately 90 percent of cases caused by a persistent HPV infection.
Substantial Reductions in Pre-Cancer and Safety Confirmed
The research, which examined data from over 132 million patients, also found 'substantial reductions' in precancerous cervical lesions among vaccinated individuals. This is crucial, as these lesions are a direct precursor to the disease, meaning the vaccine significantly reduces the risk of developing cancer in later life.
Addressing concerns often amplified on social media, the researchers stated that the vaccines were not linked to serious adverse side effects. They found no evidence connecting the HPV vaccine to conditions such as paralysis, infertility, chronic fatigue syndrome, or complex regional pain syndrome. The most common issues were minor and short-lived, like a sore arm at the injection site.
A Call for Increased Vaccination Rates
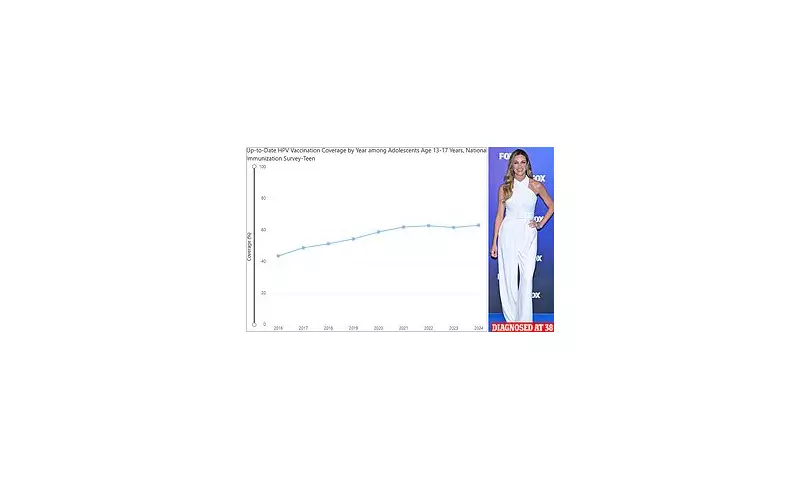
Despite the proven benefits, vaccination rates, while improving, remain below targets. In the US, 62.9 percent of adolescents aged 13 to 17 are now up to date with their HPV vaccinations, a record high but still far below the World Health Organization's target of 90 percent. Experts stress that this higher rate is needed to stop the virus from spreading within the population.
The real-world impact is already visible. In the United States, cervical cancer rates dropped by a further 11 percent between 2012 and 2021 among 20- to 24-year-olds, following the vaccine's introduction in 2006. This builds on previous declines achieved through screening programmes.
Dr Jo Morrison, a UK gynaecologist and senior author of the analyses, emphasised the broader benefits: "These reviews make it clear that HPV vaccination in early adolescence can prevent cancer and save lives. Vaccinating boys as well as girls boosts protection for everyone. Over time, we'll see the impact of vaccination on other cancers too, including ones that affect men."
With about 36,000 cancers caused by HPV every year in the US alone—including cancers of the throat, mouth, vulva, penis, and anus—the push for wider vaccination is more urgent than ever. The message from the medical community is unequivocal: this vaccine is a safe, effective, and vital tool in the fight against cancer.






