Robert F. Kennedy Jr., the Health and Human Services Secretary, has recently promoted the controversial and unproven assertion that ketogenic diets can "cure schizophrenia." While scientists strongly disagree with this characterization, emerging preliminary research does suggest that such diets might help alleviate psychiatric symptoms in some individuals.
Scientific Studies Show Symptom Improvement, Not Cure
Preliminary small-scale studies have indicated that following a ketogenic diet—a high-fat, low-carbohydrate regimen that induces ketosis in the body—could benefit people living with mental health conditions like depression, schizophrenia, and bipolar disorder. A Stanford University study involving 21 participants taking medication for bipolar disorder or schizophrenia, who were placed on the keto diet, found that a majority experienced "clinically meaningful improvement" in their psychiatric symptoms.
Furthermore, a study published in the Journal of the American Medical Association (JAMA) observed "modest improvements" in depression symptoms among individuals adhering to a keto diet. A notable 2019 case study, which Kennedy appeared to reference, documented two people with schizophrenia who were able to discontinue antipsychotic medications while following the diet.
Researchers Caution Against Overstatement
However, Dr. Christopher Palmer, who contributed to the 2019 paper, clarified that Kennedy's claims about a cure are "not accurate" and emphasized the need for further research. "Although I appreciate Secretary Kennedy's enthusiasm for my work, I have never claimed to have cured schizophrenia or any other mental disorder, and I certainly never use the word 'cure' in my work," Palmer told the New York Times.
Palmer's study revealed that the two patients who maintained the diets could manage their symptoms effectively, but they appeared to be outliers compared to others who did not achieve similar outcomes. "It's unfortunate that he used the word cure," Palmer remarked to the Harvard Crimson. "If he had simply said powerful treatment, it would have been spot on."
Lack of Conclusive Evidence and Potential Risks
For years, researchers have hypothesized a potential link between psychiatric symptoms and metabolic issues, partly based on studies of medication-resistant epilepsy in children. Nonetheless, no "gold-standard" scientific studies have been conducted on adult psychiatric patients to confirm these suspicions. Preliminary investigations are often limited in scale and typically lack control groups of individuals following non-keto diets.
Ken Duckworth, the medical director of the National Alliance on Mental Illness, commented to the Washington Post, "There's a germ of truth here. But the science is not sophisticated yet."
Kennedy's Health Agenda and Concerns
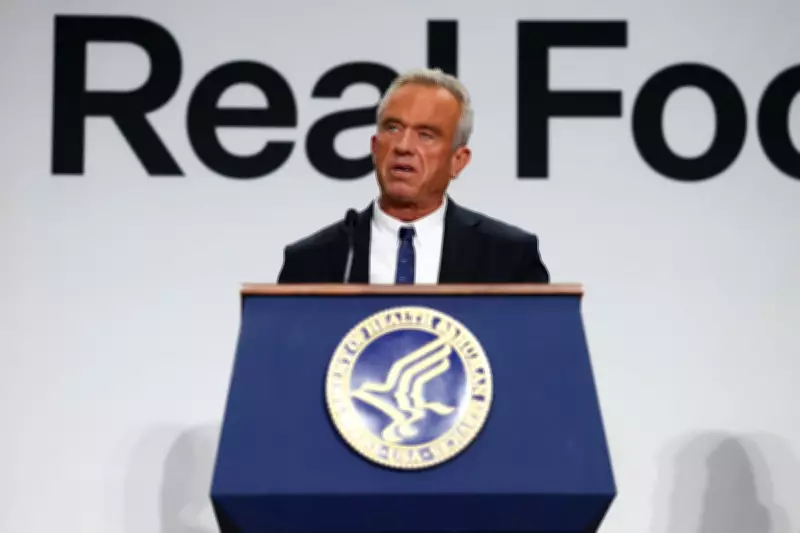
Earlier this month, Kennedy asserted that Palmer's research demonstrated keto diets could "cure schizophrenia" while promoting his "Eat Real Food" initiative. Kennedy has advocated for healthier eating habits among Americans, recommending a reduction in processed food consumption. His revised food pyramid encourages increased intake of meat and saturated fats, such as whole milk and cheese.
Palmer expressed concerns that Kennedy's unfounded claims might mislead individuals with schizophrenia into stopping their medication and adopting a keto diet without medical supervision. "That would be catastrophic," Palmer warned the Harvard Crimson, highlighting the potential dangers of such actions.
The Independent has reached out to the Department of Health and Human Services for comment on these matters, underscoring the ongoing debate between political rhetoric and scientific evidence in public health discourse.





