Scientists have issued a stark warning that lingering symptoms of Covid-19, such as persistent brain fog, headaches, and changes to smell or taste, could be a marker for an increased risk of developing Alzheimer's disease in later life.
The Tau Protein Connection
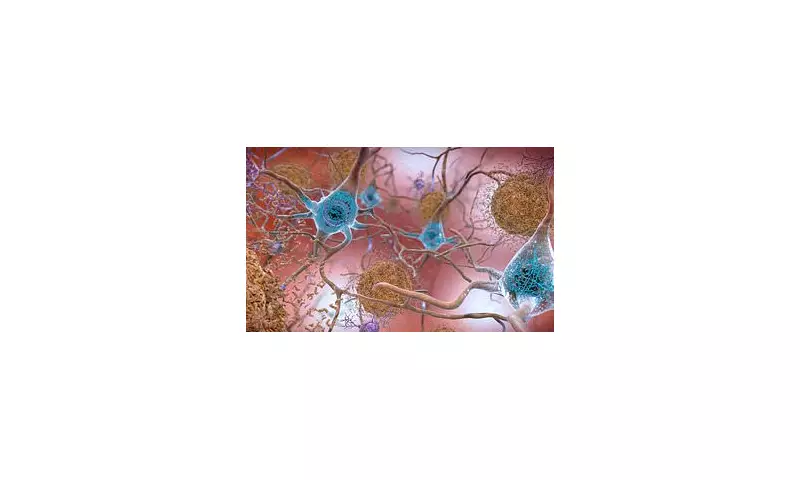
Researchers in the United States made the discovery after analysing blood samples from more than 225 patients suffering from long Covid. They found significantly elevated levels of tau, a protein intimately linked to the development of Alzheimer's and other forms of dementia. In these neurodegenerative diseases, abnormal clumps of tau form tangles inside the brain's nerve cells, disrupting communication and driving the characteristic memory loss and cognitive decline.
The study, published in the journal eBioMedicine, focused on a specific, abnormal subtype of tau known as pTau-181, which is strongly associated with Alzheimer's pathology. The team analysed samples from 227 participants in the World Trade Center Health Program, a long-running cohort of 9/11 first responders. Crucially, they had blood from before the individuals contracted Covid and again an average of 2.2 years after infection.
Significant Rise in Key Biomarker
The results were telling. Overall, participants showed an almost 60 per cent rise in blood tau levels after Covid if they experienced neurological symptoms like headaches, vertigo, or brain fog. Furthermore, those whose cognitive symptoms persisted for more than 18 months had significantly higher levels of these tau biomarkers than those whose symptoms resolved sooner.
Dr Benjamin Luft, an infectious disease expert and the study's lead author, stated: 'The long-term impact of Covid-19 may be consequential years after infection and could give rise to chronic illnesses, including neurocognitive problems similar to those seen in Alzheimer's disease.' He emphasised the practical implications for developing effective vaccines and therapies to prevent acute infection before it can embed itself and lead to long-term disease.
Professor Sean Clouston, a preventive health expert and co-author, noted: 'Elevated tau in the blood is a known biomarker of lasting brain damage. These findings suggest long Covid could worsen over time, causing neurological symptoms or cognitive difficulties that progressively intensify.' However, he cautioned that it is not yet known whether the increase follows the same biological trajectory as in those who develop Alzheimer's.
Implications for Public Health
The team compared their findings with a control group of 227 World Trade Center responders who either never had Covid or had the infection without developing long-term symptoms. Unlike the long Covid group – also known as neurological post-acute sequelae of Covid (N-PASC) – this control group showed no significant rise in blood tau.
The authors acknowledged that their cohort, comprised of essential workers with potentially greater viral exposure, may not be fully representative of the wider population. Nevertheless, they described the work as among the first to suggest a virus may contribute to abnormal tau production over time, with important implications for understanding the pathways to neurodegenerative disease.
According to NHS England survey data, nearly one in ten people believe they may have long Covid, where symptoms persist for more than 12 weeks. Office for National Statistics figures indicate around 3.3 per cent of people in England and Scotland – roughly two million – were experiencing symptoms, with 71 per cent reporting they had lasted at least a year. More than half said symptoms persisted for two years or longer.
In the UK, Alzheimer’s disease currently affects around 982,000 people, a figure projected to rise to 1.4 million by 2040. The researchers' next step is to validate their findings using neuroimaging to see if rising blood tau levels correspond to increased tau accumulation in the brain, which would provide stronger evidence of a direct link to neurodegenerative conditions.