The ongoing debate about legalising kidney sales in the UK has sparked intense discussion among healthcare professionals and ethicists, with many arguing that financial incentives would fail to address the fundamental issues within the transplant system.
The Current Transplant Crisis
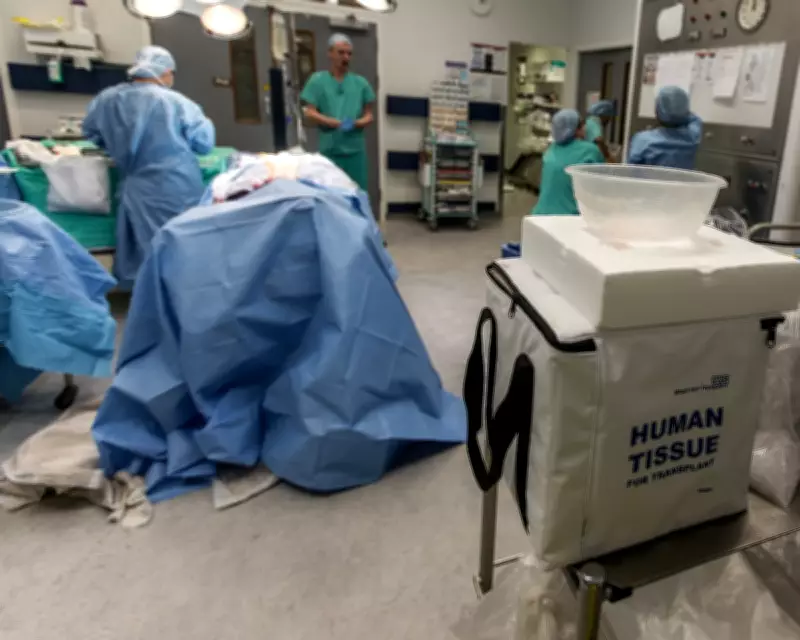
Approximately 7,000 people in the United Kingdom are currently waiting for a kidney transplant, with six individuals dying each week while on the waiting list. Despite this urgent need, only 3,302 adult transplants were performed in the 2024/25 period, creating a significant gap between supply and demand that continues to cost lives.
Questioning the Market Solution
Recent arguments advocating for legalised kidney sales have been met with scepticism from healthcare experts who question whether financial incentives would genuinely solve the underlying problems. Sandra Currie, Chief Executive of Kidney Research UK, expressed concern that such proposals accept late diagnosis and progression to kidney failure as inevitable rather than addressing prevention strategies.
The ethical implications of creating a market for human organs remain deeply troubling, particularly regarding potential exploitation of economically vulnerable individuals. As Currie notes, "How can a system be just if it starts to depend on people under financial pressure selling their organs and allowing economic vulnerability to become the engine of organ supply?"
Untapped Altruistic Potential
Contrary to arguments suggesting altruism has reached its limits, research indicates significant untapped willingness among the British public to donate kidneys voluntarily:
- More than half of UK adults would consider donating to a family member
- Nearly one third would consider donating to a friend
- One in seven would consider donating to a stranger
- Over two-thirds express desire to make positive impact even at personal cost
The challenge lies not in public unwillingness but in effectively informing and supporting potential donors through existing ethical frameworks.
Learning from International Examples
Proponents of kidney markets often cite Iran's system as evidence of success, but closer examination reveals significant limitations. Recent studies indicate that despite Iran's market approach, only 2,500 transplants occur annually from approximately 32,000 dialysis patients, with just 40% coming from living donors.
Dominique E Martin, Professor in Health Ethics at Deakin University, notes that "eliminating a waiting list is easy; one need only restrict the eligibility criteria for wait-listing." The Iranian waiting list continues to grow due to better patient identification and increasing kidney disease prevalence, suggesting market solutions don't address root causes.
Systemic Challenges Within the NHS
Beyond ethical considerations, practical barriers within the NHS transplant system present significant obstacles. One anonymous former potential donor described their experience as "a shambles and so disheartening" that they abandoned their application without follow-up from the health service.
Another donor attempting to help a friend reported "huge delays" and "incompetent" handling of their case, highlighting administrative challenges that may be contributing to the transplant shortage as much as donor availability.
A Comprehensive Approach Needed
Experts argue that sustainable solutions require multi-faceted approaches rather than reliance on financial incentives:
- Increased investment in kidney disease prevention and early detection
- Improved public awareness about kidney health and donation options
- Enhanced support systems for living kidney donors
- Addressing healthcare inequalities affecting kidney disease diagnosis and treatment
- Streamlining NHS transplant processes and reducing administrative barriers
As Sandra Currie concludes, "Saving lives doesn't mean monetising our organs. It demands investment in prevention, research, fair access to transplantation, and sustained support for ethical, voluntary donation."
The debate continues as healthcare professionals, ethicists, and policymakers grapple with balancing urgent transplant needs against ethical principles and systemic healthcare challenges within the UK's National Health Service.





