Alarming Glaucoma Figures Reveal Growing UK Health Crisis
Startling new research has uncovered that more than one million people across the United Kingdom are currently living with glaucoma, a leading cause of irreversible blindness. The comprehensive analysis, published today, paints a concerning picture of an escalating public health challenge that experts warn will intensify dramatically in the coming decades.
Projected Surge and Demographic Drivers
According to detailed projections from the Institute of Ophthalmology, the number of individuals aged over 40 affected by this debilitating eye condition could swell to over 1.6 million by the year 2060. This represents a staggering 60 per cent increase from current levels. The research, published in the British Journal of Ophthalmology, indicates that previous estimates of around 700,000 cases significantly underestimated the true scale of the problem, failing to account for the nation's evolving demographic profile.
The anticipated surge is driven by a combination of an ageing population and growth within higher-risk ethnic groups. The risk of developing glaucoma rises sharply with age, affecting approximately 11 per cent of those aged 85 and over. Researchers analysed official population data from the 2021–22 census, focusing on 34 million adults aged 40 and above, as the condition is rare in younger people.
The Silent Threat and Diagnostic Failures
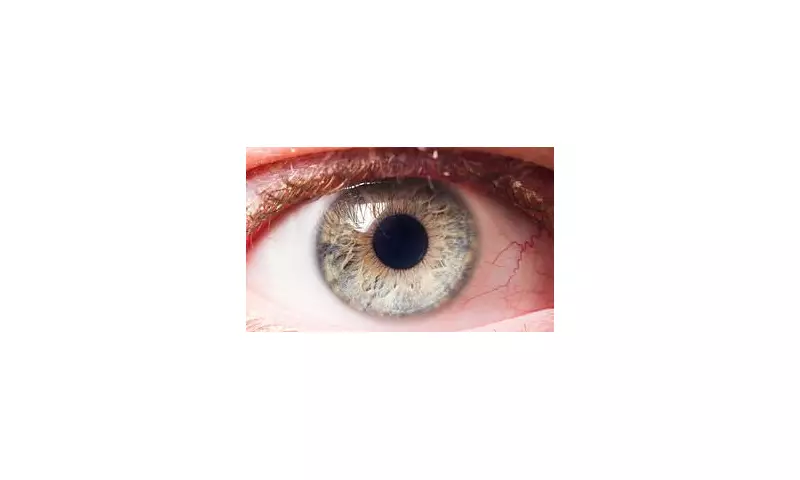
Glaucoma develops when pressure builds inside the eye, damaging the optic nerve that transmits visual information to the brain. It is most prevalent in people over 50 and is notoriously insidious, often presenting no noticeable symptoms until significant, permanent vision loss has already occurred.
This silent progression contributes to a critical diagnostic gap. The study cautions that the real number of cases is likely far higher than the estimated 1,019,629, with more than half of all glaucoma cases believed to be undiagnosed. Even within well-resourced healthcare systems, approximately 50 per cent of cases remain unidentified. This gap is particularly pronounced among ethnic minority communities, who face greater delays in diagnosis and are more likely to present with advanced disease.
Dr Laura Antonia Meliante, lead author from the Institute of Ophthalmology, emphasised the implications: 'These demographic shifts are anticipated to amplify the burden of glaucoma on the healthcare system over the forthcoming decades, underscoring the need for long-term healthcare planning to address growing demand.'
Urgent Calls for Public Health Action
Eye experts involved in the research state the findings 'underscore the need for targeted public health strategies'. They warn that more than 40 per cent of patients in the UK suffer preventable vision loss due to late diagnosis. In a commentary accompanying the study, specialists Dr Alexander Schuster and Dr Cedric Schweitzer described an urgent prevention gap.
'This increase underlines a critical need for strategies that go beyond treatment options, focusing on evidence-based healthcare planning, including structured case detection and treatment to prevent blindness at old age,' they stated. 'It is now time to take action by scientifically developing and evaluating these strategies.'
They highlighted promising evidence from a recent Swedish trial suggesting that population-wide screening at age 67 could halve the number of people who lose their sight to glaucoma.
Risk Factors and Current Recommendations
While the exact cause of glaucoma is not always known, key risk factors include being over 50, having a close family member (parent, sibling) with the condition, or having other medical issues such as diabetes. The study found rates were slightly higher in men, with the highest prevalence observed in African ethnic groups and the lowest in Asian populations.
Most cases are detected during routine eye examinations, often before symptoms manifest. Consequently, the NHS advises adults to have an eye test at least every two years, with more frequent checks recommended for those at higher risk. Although there is no cure, early intervention with treatments like eye drops, laser therapy, or surgery can slow disease progression and prevent further sight loss.
Broader Implications and Future Outlook
The lifetime visual prognosis for patients remains a major concern, with up to 16 per cent developing blindness in both eyes by the end of their lives. The researchers concluded that accurately identifying those at highest risk of progression is paramount, alongside implementing effective long-term management strategies.
The financial and societal burden is substantial. Sight loss is estimated to cost the UK economy approximately £58 billion annually through lost productivity and increased pressure on NHS and social care services. Furthermore, vision impairment is linked to a higher risk of developing dementia.
Dr Meliante summarised the imperative for action: 'Accurate, up-to-date estimates and long-term projections are therefore essential for the development and implementation of viable preventative strategies, including public awareness campaigns aimed at reducing delays in diagnosis and treatment.' The findings present a clear mandate for strengthened routine eye checks and a renewed focus on preventative healthcare planning to mitigate this growing crisis.





