Sickle Cell Patients Fear for Lives as Vital NHS Unit Faces Closure
Patients living with sickle cell disease are fighting to save a specialist NHS day unit they rely on during agonising pain crises, warning that its closure will force them into general Accident and Emergency departments where delays and inadequate care could have fatal consequences. The specialist Sickle Cell Day Unit at the Royal London Hospital is set to close on January 30 following a temporary six-month trial, sparking widespread alarm among the community it serves.
'Treated Like Junkies': The Stark Reality of A&E for Sickle Cell Patients
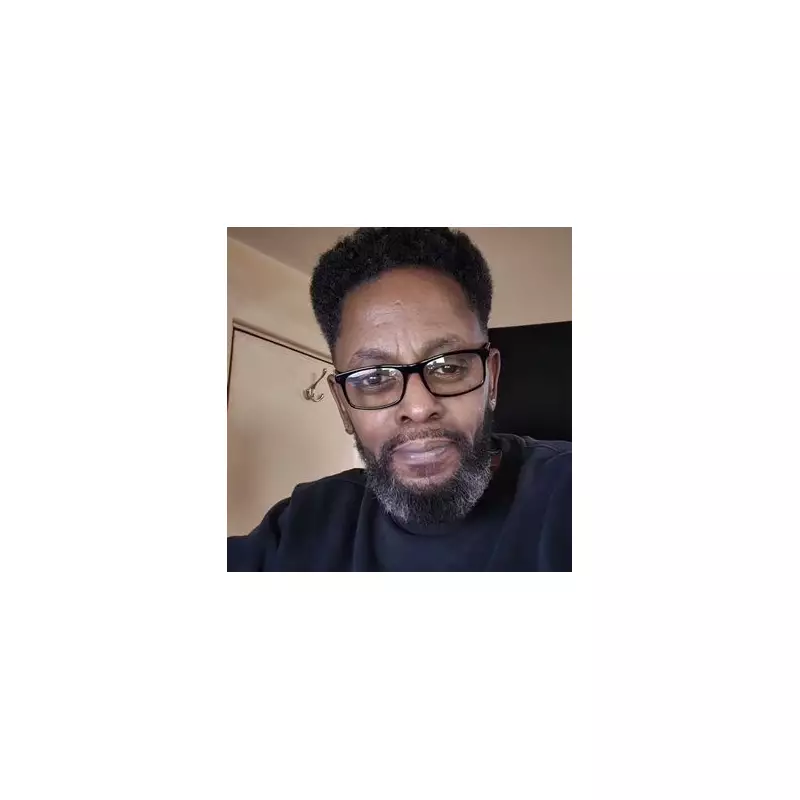
Delo Biye, a 48-year-old London sickle cell patient who launched a petition that has garnered over 24,000 signatures, describes a harrowing contrast between the specialist unit and standard A&E care. "We don't want to go [to A&E], because you can be there in a lot of agony and could take 12 plus hours before you get a bed - it's too much," he told the Mirror. "And on top of that, you have to chase to get treatment."
In the specialist unit, Delo explains, "There are usually three nurses minimum and they're dedicated to you, they understand the condition and get the medication to you on time. In A&E you're already in pain and you've got to actually start looking for a nurse."
This sentiment is echoed by Calvin Campbell, a 61-year-old sickle cell patient and NHS Senior Community Ambassador, who reveals the distressing stigma often faced in hospitals. "We aren't shocked because we know how bad the treatment can be, we've been telling you for years, we're not treated very well. We're treated like junkies. I've been called a junkie just because I asked for a prescription."
A National Pattern of Specialist Service Erosion
The Royal London unit is not an isolated case. Nationally, there are just seven emergency specialist sickle cell services similar to it. NHS England has been running a two-year pilot of emergency department bypass units, with the scheme now under evaluation as these pilots conclude. Meanwhile, the Royal London service faces imminent closure, raising concerns about a wider, quiet scaling back of specialist provision despite rising demand.
John James, CEO of the Sickle Cell Society, which backs Delo's petition, states: "Tragic cases have shown the real consequences when emergency care fails. Time and time again we hear from people with sickle cell who delay going to A&E because they fear not being believed, and inadequate treatment that might put their lives at risk."
Historical Tragedies and Unheeded Warnings
In 2021, an All Party Parliamentary Group inquiry report titled No One's Listening was published following the death of 21-year-old Evan Nathan Smith in 2019 at North Middlesex Hospital. Evan died after staff delayed treatment during a sickle cell crisis, lacked understanding of the condition, and refused him oxygen. He even called 999 from his hospital bed, but the emergency operator spoke to ward nurses and decided not to dispatch paramedics.
Despite this damning report, tragedies have continued. In 2023, 30-year-old Dave Onawelo died in hospital after attending A&E struggling to breathe. He told staff he believed he was having a sickle cell crisis, but a nurse deemed him not acutely unwell. A senior nurse later refused to help him, stating she was 'busy with six patients.' A coroner found the Trust failed to recognise a critically ill patient with a pre-existing condition and that a lack of compassion and clinical curiosity contributed to the preventable death.
The Fight for Specialist, Sustainable Care
The Sickle Cell Society warns that people with sickle cell have long been failed by emergency care that does not meet their needs. The charity argues the Royal London pilot demonstrated what is possible when care is specialist, timely, and prioritised, and is calling on the NHS to commit to sustained funding for such services.
"We believe decisions of this nature about healthcare service provision should be informed by clear evaluation data, showing what delivers the best outcomes for patients and supports healthcare professionals," a spokesperson said.
Petition organiser Delo remains defiant, questioning the authorities' responsiveness. "What does it take for them to budge? What does it take to actually hear the people that you're supposed to be treating? There's over 20,000 petitions saying that there is a need."
NHS Trust Response and Patient Fears
Barts Health NHS Trust, responding to the petition, confirmed the unit will close at the end of January. A spokesperson stated: "Funded by the North East London Integrated Care Board, it involved testing an alternative route for treating emergency patients with sickle cell disease who were experiencing acute pain. This was alongside the normal route of being treated through our A&E. There is no change to the way we manage patients with sickle cell disease, and our Haematology Day Unit remains open for all our elective transfusion therapies. Patients with sickle cell disease will continue to receive specialist-led care at our hospital."
However, patients and families fear this represents a dangerous step backwards, exacerbating long-standing inequalities in care for a condition that disproportionately affects people of African or Caribbean heritage. They argue that losing this dedicated, understanding environment will inevitably lead to more suffering and potentially more preventable deaths in overstretched, under-informed general A&E settings.





