For millions of women in the UK, a cough, a sneeze, or a jog can lead to an embarrassing and distressing reality: stress urinary incontinence (SUI). Many suffer in silence, believing, as one woman did for years, that it's simply the price of motherhood, ageing, or failing to do enough pelvic floor exercises. But a personal journey reveals a startling gap in women's healthcare knowledge and a life-changing treatment option that remains shrouded in silence.
The Silent Suffering: A Story Shared by Millions
The author's story begins with a legacy of incontinence, watching her active mother eventually abandon running for hiking. She internalised the common refrain: "I should have done more Kegels." Years later, after her own pregnancies, she faced the same fate. Simple acts like coughing while walking necessitated a change of underwear. The well-meaning advice from friends was always the same: "Have you done your Kegels?"
This experience is far from unique. Research indicates that 45% to 50% of women experience SUI at least once a week. Yet, a profound communication chasm exists in healthcare; for every case reported to a GP, an estimated 20 go unreported. The author, like so many, never mentioned her symptoms during medical appointments, and crucially, no healthcare professional ever asked. She resigned herself to a life limited by black leggings and carried tissues, believing her condition was a personal failing.
A Turning Point and the Discovery of Options
The breaking point came in early 2024, following a long run and a church service where a pervasive odour turned out to be her own. That evening, a simple sneeze resulted in another accident. Enough was enough. She contacted a specialist bladder and pelvic health centre, setting in motion a revelation.
In consultation with her doctor, she was presented with four main treatment avenues:
- Pelvic Floor Muscle Training (PFMT): Beyond basic Kegels, but requiring significant, consistent effort.
- The Poise Impressa: A temporary, tampon-like device for urethral support.
- Bulking Agent Injections: A minimally invasive procedure where a substance is injected into the urethral tissue to create a better seal.
- The Sling Surgery: A gold-standard, more invasive surgical option creating a supportive "hammock."
Having struggled with consistent Kegels and needing a lasting solution that didn't involve major surgery or recovery time, she opted for the bulking agent procedure.
The Life-Altering Procedure: Quick, Effective, Underutilised
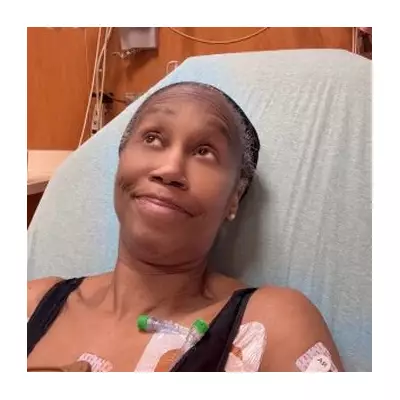
The treatment, performed in a doctor's office, involved a series of injections after local anaesthetic. While briefly uncomfortable, it was comparable to other minor aesthetic procedures. The result was transformative. The very next day, she ran without a single leak. A minor top-up injection a month later perfected the results.
The physical freedom was profound. She realised she had unconsciously altered her gait and posture to minimise leakage. Her running times improved, matching her high school personal bests. Within a year, she completed seven trail half-marathons. Most tellingly, her doctor examined her and stated, "Your pelvic floor is actually really strong. No amount of Kegels was going to fix this for you."
The Systemic Failure in Women's Health Knowledge
This is where the core issue lies. The author's journey took years, not due to a lack of effective treatment, but due to a catastrophic failure of information dissemination. Bulking agents are not new; they were first used in the 1930s, with significant innovations in the late 1980s. Modern agents like Bulkamid (approved by regulators in 2020) can offer relief for many years.
Yet, studies suggest less than 15% of women bothered by SUI receive an injection or surgery. Anecdotally, every person the author told was unaware such treatments existed. The narrative remains dominated by Kegels and behavioural modifications—lose weight, cut caffeine—which can inadvertently shame women, implying their suffering is their own fault.
This stands in stark contrast to how society approaches men's quality-of-life health issues. Furthermore, disparities in research funding and female inclusion in clinical trials persist. The combination of stigma, outdated assumptions, and a lack of proactive discussion in healthcare settings leaves millions of women needlessly limiting their lives.
The author's conclusion is clear: SUI is not an inevitable part of ageing or motherhood, and it is not solely a matter of pelvic floor weakness. A range of effective, minimally invasive treatments exist. The urgent need is for greater awareness, open conversation between patients and healthcare providers, and a systemic shift to ensure every woman knows that she does not have to just "deal with it."