A common and often easily treated infection is becoming an increasing challenge for healthcare professionals and patients alike. Thrush, caused primarily by the yeast Candida albicans, is developing resistance to the antifungal drugs used to combat it, leading to fewer effective treatment options.
The Growing Threat of Antifungal Resistance
For decades, the antifungal drug fluconazole has been the first-line treatment for most Candida infections, including thrush. However, the landscape is shifting rapidly. According to the US Centers for Disease Control and Prevention, about 7 per cent of all Candida blood samples tested now show resistance to fluconazole.
This resistance is not static. Research indicates a clear upward trend over at least the past eight years. A recent study from Egypt presented an alarming snapshot, finding that in 2024, nearly 26 per cent of Candida albicans isolates from blood samples were resistant to fluconazole. While more global data is needed, the direction of travel is concerning.
The consequences are twofold. Firstly, routine thrush infections are becoming more difficult to manage. Secondly, and more seriously, severe systemic Candida infections—which can occur in immunocompromised individuals or those on long-term antibiotics—are becoming harder to control. This resistance is also implicated in the rise of recurrent thrush, a condition affecting around 138 million women worldwide, a figure projected to climb to 158 million by 2030.
Why Are the Fungi Adapting?
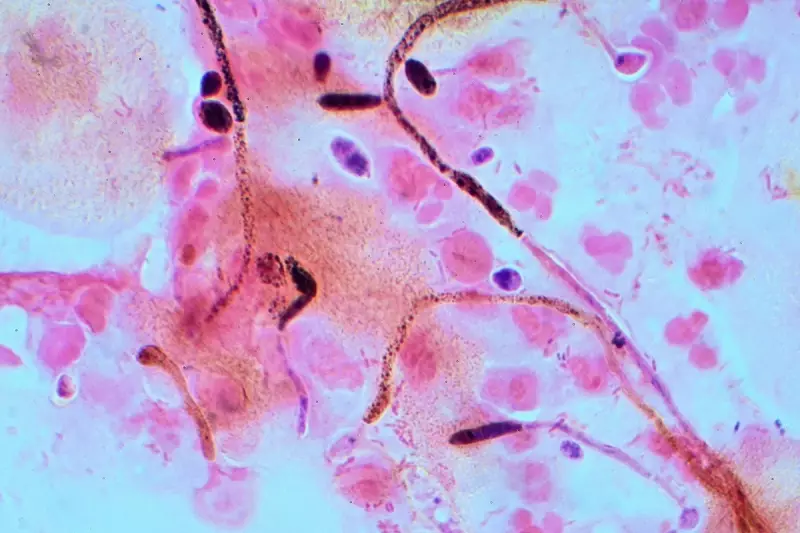
Candida albicans is a highly adaptable organism. It employs several sophisticated strategies to survive antifungal assault. These include genetic mutations that reduce drug susceptibility, the ability to alter the drug's target molecules, and the formation of resilient biofilms.
These slimy, protective layers of fungal cells act as a formidable barrier. They block drug entry, actively pump out any drugs that penetrate, and allow some cells to enter a dormant state, only to re-emerge once treatment ends.
This resistance is not occurring in a vacuum. Key drivers include the misuse and overuse of antifungal drugs in both human medicine and agriculture. Furthermore, the pipeline for new antifungal medications is limited, as they are notoriously difficult and expensive to develop.
Environmental pressures are also playing a role. Increasing temperatures, ecological stress, and widespread fungicide use are creating conditions that favour the emergence of hardy, drug-resistant strains. A prime example is Candida auris, a multi-drug resistant fungus that poses a severe threat in healthcare settings.
Protecting Yourself and Preventing Spread
Maintaining a healthy immune system and a balanced microbiome is the first line of defence. The beneficial bacteria in our bodies naturally keep Candida populations in check. Disruption from antibiotics, a poor diet, high stress, or illness can allow the yeast to overgrow.
To support your microbiome, experts recommend a diverse, fibre-rich diet that includes fermented foods, while limiting highly processed items. Only take antibiotics when absolutely prescribed by a doctor, and consider probiotics, especially after a course of antibiotics.
In terms of transmission, Candida primarily spreads through direct person-to-person contact, sexual contact, and contaminated surfaces or objects. In hospitals, it can spread via medical equipment. While airborne transmission is not considered common, a recent study from Hong Kong detected drug-resistant Candida species, including Candida albicans, in urban air samples. This potential new exposure route, particularly in crowded spaces or healthcare environments, requires further investigation.
Everyone can contribute to slowing resistance. Only use antifungal medicines as prescribed and always complete the full course. Practising good hygiene also helps reduce the risk of infection and spread. By understanding the causes and adopting preventive measures, the public and medical professionals can work together to address this growing health concern.





