RFK Jr's Controversial Claim on Keto Diet and Schizophrenia
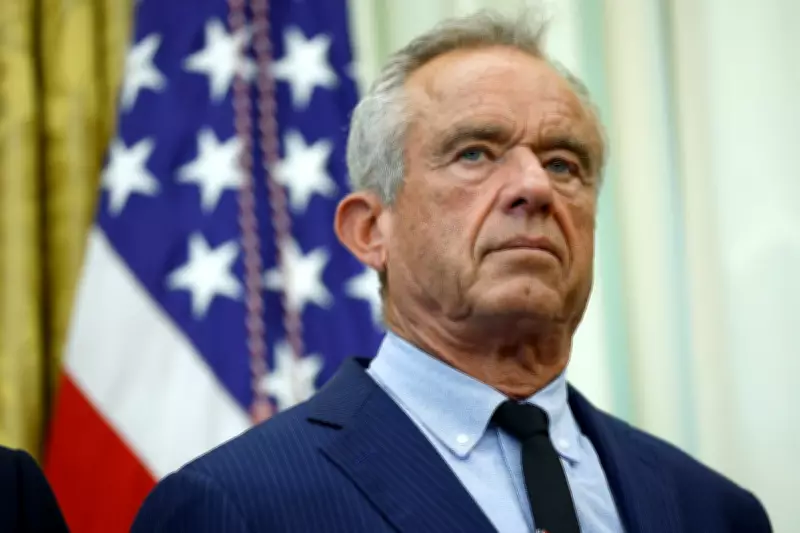
Health and Human Services Secretary Robert F. Kennedy Jr. made an unfounded assertion on Wednesday that the ketogenic diet can cure schizophrenia, prompting immediate backlash from health professionals who described the comment as a significant overstatement regarding the diet's relationship with the mental disorder.
Tour Promotes New Dietary Guidelines
Kennedy delivered these remarks while visiting Tennessee as part of a national tour aimed at encouraging Americans to "eat real food," according to reports from The New York Times. This tour functions as an informational campaign to highlight recent changes he has implemented to federal dietary guidelines. The updated recommendations advocate for increased consumption of protein and fats—such as steak, cheese, and butter—alongside whole milk, while advising against carbohydrates.
During his appearance at the Tennessee State Capitol, Kennedy stated, "we now know that the things that you eat are driving mental illness in this country," and claimed that a Harvard doctor had "cured schizophrenia using keto diets." He further referenced studies he had seen recently, saying, "There are studies right now that I saw two days ago where people lose their bipolar diagnosis by changing their diet."
Health Experts Challenge the Assertion
Health experts were quick to dispute Kennedy's claims, emphasizing the lack of credible evidence supporting such a cure. Dr. Paul S. Appelbaum, a professor of psychiatry at Columbia University and former president of the American Psychiatric Association, told The New York Times that it is "simply misleading" to suggest schizophrenia symptoms can even be improved by the keto diet, let alone cured.
Dr. Mark Olfson, another Columbia psychiatry professor, echoed this sentiment, stating, "There is currently no credible evidence that ketogenic diets cure schizophrenia." He pointed out that most studies examining the keto diet as a treatment for mental health disorders, including a Stanford study referenced by Kennedy, lacked control groups following regular, non-keto diets, which undermines their reliability.
Background on Kennedy's Dietary Advocacy
Kennedy's endorsement of the keto diet for treating mental illnesses follows his declaration in January that the "war on protein" and "war on saturated fats" had ended. On January 7, he proclaimed, "Today the lies stop. Protein and healthy fats are essential and were wrongly discouraged in prior dietary guidelines."
The Health and Human Services Secretary has a history of skepticism toward conventional medical practices. In 2024, he asserted that ADHD medication had "poisoned" an entire generation of children. Last year, he dismissed the entire 17-member Centers for Disease Control and Prevention Advisory Committee on Immunization Practices vaccine board, replacing them with handpicked skeptics.
Understanding the Keto Diet
The ketogenic diet, commonly referred to as "keto," typically involves at least 70 percent of calories derived from fat, fewer than 10 percent from carbohydrates, and fewer than 20 percent from protein. It has gained popularity for weight loss without requiring a vegan lifestyle or severe caloric reduction. However, critics warn that its heavy focus on fats may pose long-term risks to heart health.
While many individuals report successful weight loss on the keto diet, adherence can be challenging due to restrictions on numerous foods, including common staples like certain fruits and vegetables, as well as beloved treats such as pizza.
Research on Keto and Mental Health
In Tennessee, Kennedy appeared to reference a 2019 paper by Dr. Christopher Palmer, which described two patients with longstanding schizophrenia who experienced complete remission of symptoms after adopting the keto diet. According to the research, both patients were able to discontinue antipsychotic medications and have remained in remission for years.
Palmer and his colleagues noted in September that the keto diet represents a "promising therapeutic approach for schizophrenia." However, health experts caution that such findings are preliminary and do not equate to a cure. Short-term studies, like one published by Stanford last year, suggest the keto diet "might" benefit schizophrenia patients, but they emphasize that "might be helpful" is far from a definitive cure proclaimed by the nation's top health official.
The Independent has requested comments from both Dr. Palmer and Kennedy via the Department of Health and Human Services, but responses have not yet been provided. This incident highlights ongoing debates over dietary guidelines and their intersection with mental health treatment, underscoring the need for evidence-based approaches in public health policy.





