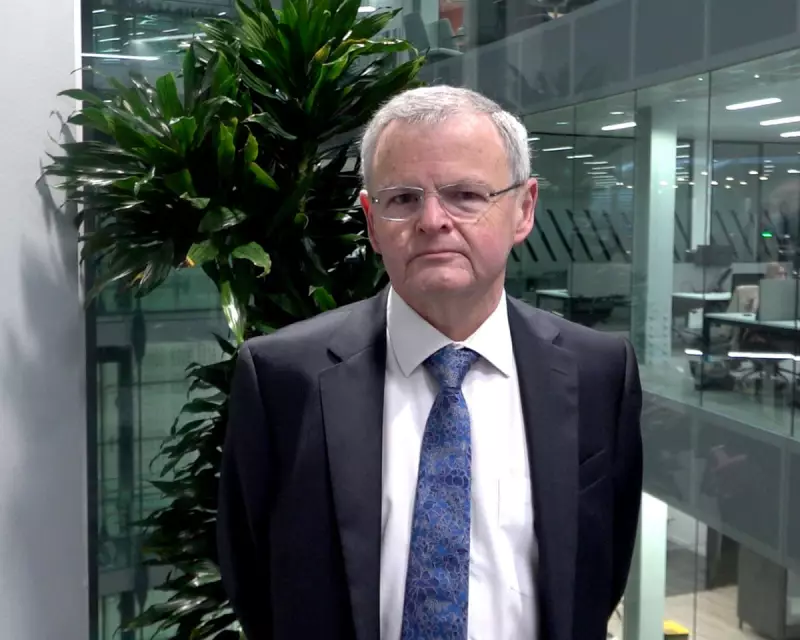
A major review of NHS adult gender dysphoria clinics in England has uncovered an "unacceptable" lack of data and projected waiting times that could stretch to 15 years for a first appointment. The inquiry, led by NHS medical director and cancer specialist Dr David Levy, found it impossible to judge the safety or effectiveness of treatments due to a systemic failure to record patient outcomes.
Critical Failings in Data and Safety
Dr Levy and his team visited nine NHS England clinics, interviewing staff and patients. The report concluded that the services' failure to study outcomes for their patients made any assessment of safety unfeasible. "Virtually no other data" beyond waiting times was available from the adult clinics, the review stated.
This absence of information means clinicians, patients, and health service commissioners cannot understand which treatments—from cross-sex hormones to psychological support—deliver the best results. The review also heard that some patients expressed regret or dissatisfaction after treatment, with a smaller number choosing to reverse their gender transition. However, the proportion who detransition remains unknown due to the data vacuum.
Exploding Waiting Lists and Patient Risks
With the number of people seeking treatment rising significantly, the average wait for a first assessment is already five years and seven months. The review projects this could reach 15 years without urgent improvements.
These extreme delays are creating serious safety issues, driving vulnerable patients to self-source hormone drugs from high-risk online providers abroad. Clinicians reported that by the time patients are seen, it is often challenging to provide appropriate support because many have already sought information—sometimes inaccurate—from online sources during the lengthy wait.
A Changing Patient Profile and Staff Concerns
The profile of referrals has shifted dramatically. The majority (57%) are now for people aged 18-25, a change from a previously older cohort. The population has also shifted from mostly birth-registered males to a more even ratio of birth-registered females, though precise data is hampered as not all clinics record sex at birth.
The review was told this younger cohort has a higher prevalence of additional conditions like autism spectrum disorder and other issues such as mental health conditions or a history of trauma. Furthermore, only 31.5% of patients were discharged having completed treatment, raising questions about why others disengaged or could not be contacted.
Some staff reported a culture where raising concerns in team meetings was discouraged, and clinical curiosity was sometimes dismissed as transphobia. The report acknowledged the "hostile and polarised" debate surrounding gender care but stressed the need for robust, high-quality research and data.
Recommendations and NHS Response
Dr Levy made 20 recommendations, including a requirement for clinics to begin nationally reporting outcomes data that includes patients' birth-registered sex. From January, he will chair a new national improvement programme for adult gender services.
Professor James Palmer, national medical director for specialised services, acknowledged that "too many people are waiting far too long" and experiences of care are variable. He stated that investment has more than doubled from £16m in 2020-21 to £36m in 2024-25, with more clinics opening to reduce waits.
While campaign group TransActual welcomed moves towards more patient-centred care, it expressed concerns about plans to end self-referrals and warned that requiring a first assessment by a senior clinician could hamper efforts to cut waiting times.





