The Hidden Pain of Hidradenitis Suppurativa
You probably don't give your armpits much thought beyond daily hygiene, but this small area of skin represents one of your body's busiest intersections. Beneath the surface lies a complex network of glands, nerves and lymph nodes working constantly to regulate temperature, fight infection and even influence how others perceive your scent.
This anatomical design allows for arm flexibility while serving as a crucial passageway for blood vessels and nerves connecting limb to torso. Yet for many people, this humble underarm becomes the site of something far more troubling than body odour - a distressing, recurring condition called hidradenitis suppurativa (HS).
What Exactly Is Hidradenitis Suppurativa?
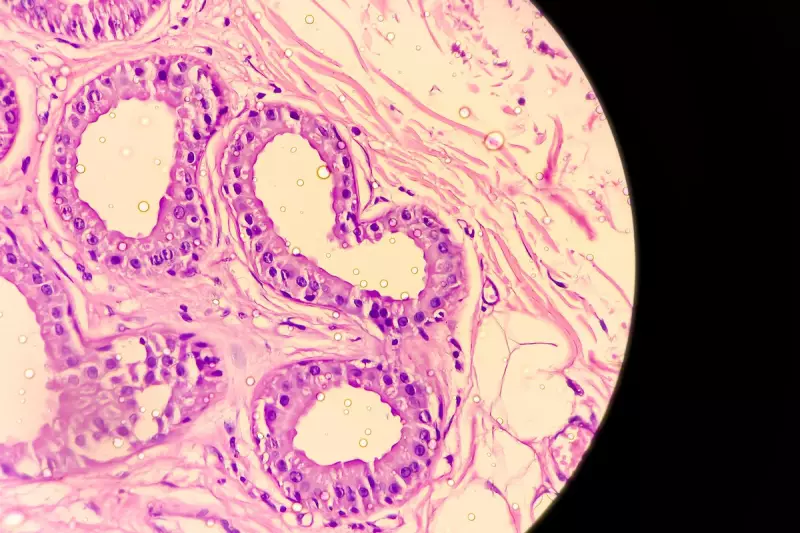
Hidradenitis suppurativa translates to 'inflammation of the sweat glands with pus', accurately describing this chronic condition. HS affects areas rich in sweat glands and hair follicles, particularly where skin folds and rubs together. While commonly appearing in armpits, it can also develop in the groin, around breasts and buttocks, and in the perineal area.
The inflammation appears driven by an autoimmune-like process where the body mistakenly attacks its own tissues. Blockage of hair follicles occurs first, subsequently triggering sweat gland involvement. Research shows the condition is nearly three times more common in women than men and often runs in families.
Other significant risk factors include increased androgen levels (hormones like testosterone that rise after puberty), smoking and obesity. Concerningly, both UK and US studies confirm that people of colour are disproportionately affected, with black and Hispanic patients experiencing more severe symptoms and diagnostic delays.
Recognising Symptoms and Seeking Treatment
Inflamed and blocked glands manifest as hard nodules or swellings on the skin. These can develop into abscesses that grow significantly in size. Prolonged inflammation leads to sinus formation - tunnels beneath the skin connecting nodules - and scarring. This can cause painful, oozing or foul-smelling skin that sometimes restricts movement when scar tissue forms.
Like common acne (which shares similar processes), HS isn't caused by poor hygiene and isn't contagious, despite widespread misconceptions. Treatment approaches often overlap with acne management, including antibiotics like lymecycline that offer both antibacterial and anti-inflammatory benefits.
Lifestyle adjustments such as wearing loose clothing and weight management to reduce skin friction are frequently recommended. In advanced cases, large abscesses measuring five to ten centimetres across may require surgical drainage or scar tissue removal. New biological therapies like adalimumab, which calm the immune system's overreaction, now help manage severe cases.
HS diagnoses increase annually, reflecting either rising incidence or improved medical recognition. The condition's variable symptoms and the embarrassment surrounding skin changes in intimate areas have historically contributed to diagnostic delays spanning years. Early detection remains crucial for preventing progression to severe disease.
The armpit might seem insignificant until hidradenitis suppurativa transforms it into a source of chronic pain that shapes daily life. Too many people endure this condition for years before receiving proper diagnosis or effective treatment. Recognising HS as a genuine medical condition rather than a hygiene issue represents a vital step toward changing this reality.





