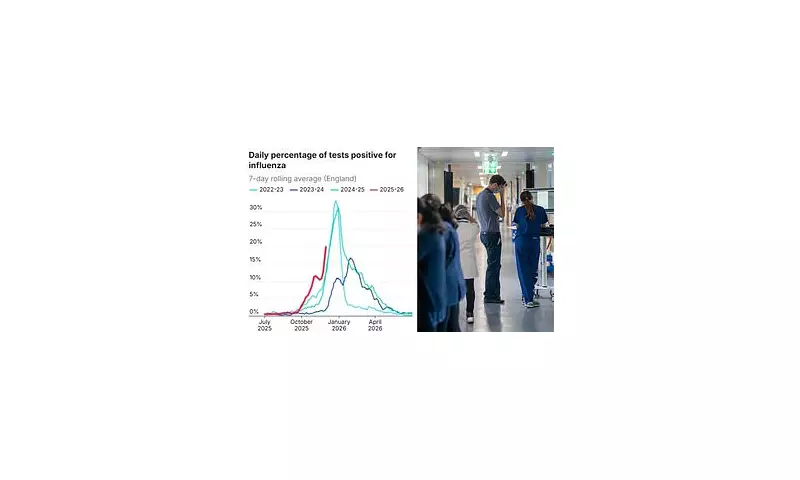
Britain is facing an unprecedented winter flu crisis, with hospital admissions hitting record highs for this time of year, driven by a rapidly spreading mutated strain. Health officials have issued stark warnings, stating there is 'no peak in sight' for the outbreak, which has already forced some hospitals in England to reintroduce mandatory mask-wearing rules.
The Dominant and Dangerous Mutant Strain
Data from the UK Health Security Agency (UKHSA) reveals that more than 80 per cent of current flu cases are now caused by a specific mutated form of the H3N2 virus, dubbed subclade K. This subtype, which was not dominant in recent years, underwent seven significant mutations over the summer, allowing it to partially evade immunity built up from previous infections or vaccinations.
Dr Mary Rodgers, a leading 'virus hunter' with Abbott's Pandemic Defense Coalition, explained the severity. 'H3N2 isn't new, but when it becomes the dominant strain, we often see more severe flu seasons,' she told the Daily Mail. 'Recent H3N2 viruses have picked up mutations that help them spread more easily or partially evade immunity. That can lead to more infections—and potentially more hospitalizations.'
Experts stress that symptoms of H3N2 are indistinguishable from other flu strains without laboratory sequencing, meaning its true circulation could be even higher than detected.
Strain on the NHS and Fears Over Vaccine Match
The impact on the National Health Service is severe and escalating. Last week, an average of 1,717 hospital beds in England were occupied daily by flu patients—a figure that is more than double the 1,098 seen at this time in 2024 and ten times higher than in 2023. Of these, 69 patients required critical care.
NHS England chief executive Sir Jim Mackey warned that flu admissions could triple or even quadruple by next week, potentially reaching between 5,000 and 8,000 occupied beds, necessitating a 'national response'. He delivered this warning amid the looming threat of a five-day junior doctors' strike from December 17, which he branded 'cruel and calculated'.
Compounding the crisis are concerns about this year's flu vaccine's effectiveness. The jab is formulated months in advance based on strains circulating in the southern hemisphere. This season's vaccine targets a version of H3N2 that predates the newly emerged subclade K. Early UKHSA figures suggest the vaccine is 70-75% effective at preventing hospital attendance in children but only 30-40% effective in adults.
Dr Antonia Ho of the University of Glasgow highlighted the danger: 'H3N2 tends to cause more severe illness than H1N1, particularly in older adults. In the 2022/23 winter season when H3N2 was dominant, there were 16,000 influenza-associated deaths, compared to 8,000 last winter.'
Public Health Response and Urgent Calls to Action
Despite questions over its match to the circulating strain, health authorities are emphatically urging eligible groups to get vaccinated. The flu jab remains the best defence against severe illness and complications. Eligible groups include those aged over 65, people with long-term health conditions, pregnant women, and carers.
There are signs the public is heeding the call, with almost 17 million flu and Covid vaccines already administered in England. The reproduction rate (R) for flu this season is estimated at 1.4, higher than the typical 1.2, indicating faster spread.
Globally, the surge has led to mask advisories in Japan and parts of the US and Spain. Dr Rodgers concluded with a sobering reminder: 'We can expect new strains to continue emerging. Even with that evolution, the flu vaccine remains one of our strongest tools for preventing severe illness.' With the NHS bracing for its toughest winter week yet, the message is clear: vigilance and vaccination are critical.