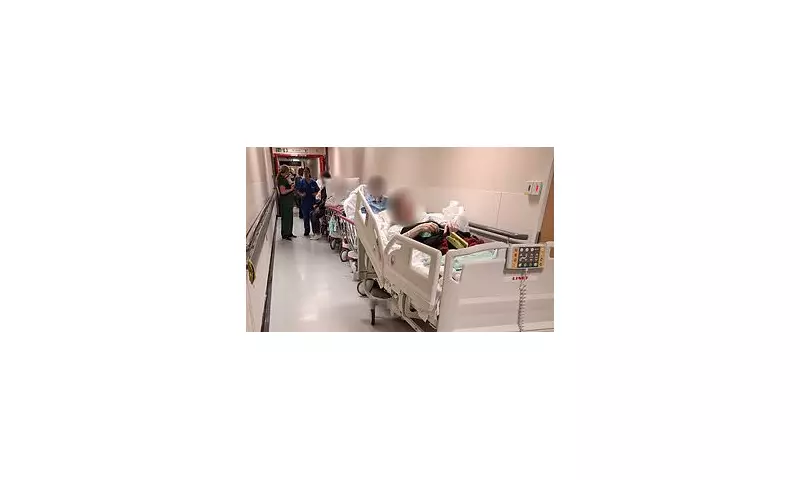
A damning internal NHS report has exposed the harrowing reality of 'corridor care' in England's hospitals, where patients are being forced to witness traumatic deaths while receiving treatment in public areas.
The Human Cost of Hospital Overcrowding
Disturbing patient testimony reveals the severe psychological impact of receiving emergency care in hospital corridors. One patient described the trauma of watching another person die just feet away from them, while others reported hearing distressing final conversations and witnessing desperate resuscitation attempts in completely inappropriate settings.
The NHS England report, based on extensive patient feedback, highlights how corridor care has become normalised despite the profound distress it causes to vulnerable individuals.
System Failure: Corridor Care Becoming Routine
Hospital bosses have admitted that corridor care is no longer an emergency measure but has become standard practice in many NHS trusts. The report indicates that patients are regularly being treated:
- In hospital corridors and public walkways
- Without privacy or dignity
- While witnessing other patients' medical emergencies
- For extended periods without proper facilities
Staff Speak Out: 'We're Failing Our Patients'
Healthcare professionals have expressed deep concern about the ethical implications of corridor care. Many report feeling compelled to provide substandard treatment due to space constraints, while others describe the moral distress of being unable to offer basic privacy to dying patients.
One senior nurse commented: "We're trained to provide compassionate end-of-life care, but in corridors we can't even offer dignity in death. It's heartbreaking for families and traumatising for other patients witnessing these events."
The Wider NHS Crisis
This corridor care crisis reflects broader systemic issues within the NHS, including:
- Chronic bed shortages and capacity issues
- Record A&E waiting times
- Staffing shortages across multiple departments
- Growing demand for emergency services
Call for Urgent Government Action
Patient advocacy groups and healthcare unions are demanding immediate intervention to address what they describe as a "national scandal." They're calling for:
- Emergency funding to increase hospital capacity
- Proper risk assessments for corridor care patients
- Mental health support for affected patients and staff
- Transparent reporting of corridor care incidents
The Department of Health has acknowledged the report and stated that reducing corridor care is a "key priority," but patients and staff await concrete action to resolve this deepening crisis.





