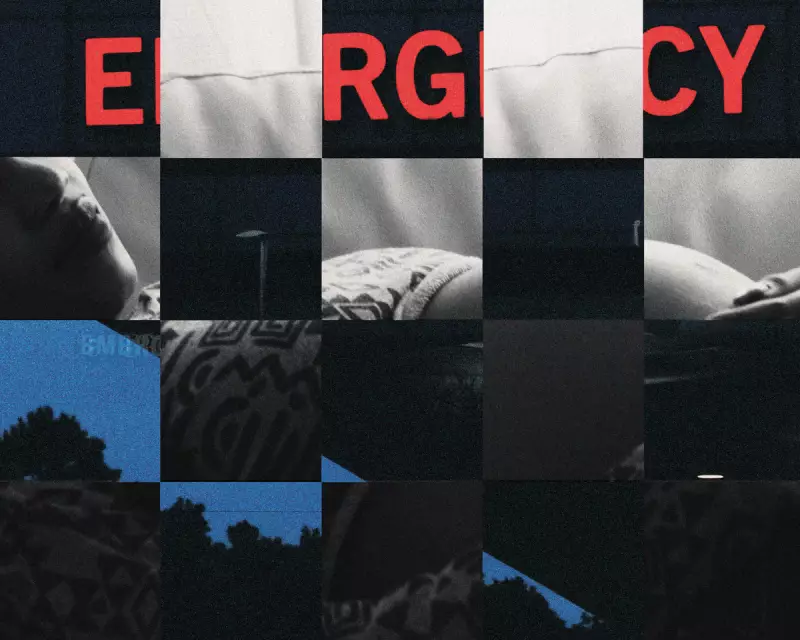
Los Angeles Maternity Crisis: Emergency Rooms Become Birthing Centres Amid Ward Closures
A growing healthcare crisis is unfolding in Los Angeles as maternity wards continue to close across the county, forcing pregnant women to seek birthing care in emergency rooms. This alarming trend is placing unprecedented pressure on hospital staff and raising serious concerns about maternal health outcomes, particularly for communities of colour.
The Rising Tide of Emergency Room Births
From 2016 to 2023, more than 26,500 individuals sought birthing care in Los Angeles County emergency rooms, with approximately 64% of these patients identifying as Latino. This represents a significant shift in how maternal healthcare is being delivered across the region. Despite a 26% decrease in births countywide during this period, emergency room visits and admissions for labour and delivery actually increased by roughly 14%.
Los Angeles County has witnessed at least five maternity ward closures since 2023, with a total of 16 units shutting down since 2014. This reduction in specialised maternity services has created a domino effect, pushing more pregnant patients toward emergency departments that are often ill-equipped to handle complex deliveries.
Healthcare Professionals Sound the Alarm
Medical staff on the front lines are expressing deep concern about this developing situation. Briah Fischer, a former resident at Los Angeles General Medical Center, emphasised the ethical dilemma facing healthcare providers: "We don't have the ability to turn patients away. And when a patient shows up, we want to take care of them because we know that they often will now have to drive an hour to two hours to the next hospital."
At Los Angeles General Medical Center, a public teaching hospital in Boyle Heights, more than 1,400 women passed through emergency room doors to access care during labour and delivery between 2016 and 2023. Sigita Cahoon, the hospital's vice-chief of obstetrics and gynecology, described working through nights to deliver multiple babies as maternity services become increasingly scarce.
Compounding Health Risks and Complications
Healthcare experts warn that this shift toward emergency room births comes with significant peril. Research into maternity ward closures nationwide demonstrates that access to prenatal care decreases when these specialised units close. Furthermore, hospitals that maintain maternity services are seeing an influx of patients with increasingly complex pregnancies.
Cahoon reported that her hospital has been treating more pregnant patients with serious conditions including high blood pressure, seizure disorders, psychiatric needs, and placenta accreta - a dangerous condition where the placenta invades the uterine wall. Angela Ocampo, who contributed to the 2025 California Equity in Maternal Health Report, highlighted additional concerns about post-natal care access for those giving birth in emergency settings.
The consequences are reflected in troubling health statistics. Los Angeles County's severe maternal morbidity rate has steadily increased in recent years, reaching 122.1 morbidities per 10,000 deliveries in 2023 - higher than the state average. Patients of colour, who face more barriers to accessing care, experience even higher morbidity rates.
Disproportionate Impact on Communities of Colour
The crisis is hitting minority communities particularly hard. From 2021 to 2023, severe maternal morbidity rates in Los Angeles County were highest among Black women, who sustained a rate of 193.5 morbidities per 10,000 deliveries. Asian/Pacific Islander and Hispanic patients followed with rates of 114.5 and 111.2 per 10,000 respectively.
Mashariki Kudumu, founder and director of the California Black Birth Equity Summit, identified systemic problems contributing to these disparities: "People are not going to get the care that they need in their communities, and so they're going to be giving birth in less ideal situations, like the emergency room."
Financial Pressures and Policy Challenges
The closure of maternity wards is driven partly by financial considerations. These units require 24/7 coverage and are comparatively expensive to operate. Hospital administrators and experts have also attributed closures to declining birth rates, increased operational costs, and shortages in labour - with California potentially facing a shortage of 1,100 obstetricians by 2030.
Medi-Cal, California's version of Medicaid, has a reimbursement rate for obstetrics below the national average despite covering almost 40% of California births. There are growing fears that federal Medicaid program cuts could exacerbate these financial pressures, potentially leading to further reductions in maternity services.
Innovative Approaches and Legislative Responses
Some hospitals are developing unique solutions to address the crisis. Martin Luther King Jr Community Hospital in south Los Angeles has been working to build a staff of midwives to address staffing concerns. The hospital, which serves a community already experiencing racial disparities in healthcare, has implemented a model where midwives provide personalised, holistic care with physician support.
Despite financial hardships that nearly prevented the hospital from paying its bills in 2023, it opened a prenatal care clinic in the same year to expand access to care throughout pregnancy. More than 3,300 women came into its emergency room in labour from 2016 to 2023, according to state data.
Legislative efforts have seen mixed results. California Governor Gavin Newsom recently signed a law enabling "standby perinatal services" to be established during a 10-year pilot period, but only at up to five rural hospitals. Other measures that would have required hospitals to notify the state of potential maternity ward closures or created standards for geographic accessibility of perinatal units failed to become law.
A Broader National Concern
While particularly acute in Los Angeles, this crisis reflects nationwide trends. More than 35% of US counties are considered maternity care deserts, largely concentrated in rural areas. Research published by the Journal of the American Medical Association shows that 537 hospitals lost their obstetric services nationwide from 2010 to 2022, with 299 of these located in urban regions.
As Laila Al-Marayati, an associate professor of clinical obstetrics and gynecology at USC's Keck School of Medicine, framed the fundamental question: "Do we as a society decide that this patient population is worth taking an extra step for because of how important it is? Are we OK with the maternal mortality rate increasing in the United States because women don't have access to good care?"
The situation in Los Angeles serves as a stark warning about the consequences of diminishing maternity services and the urgent need for comprehensive solutions to protect maternal health across vulnerable communities.





